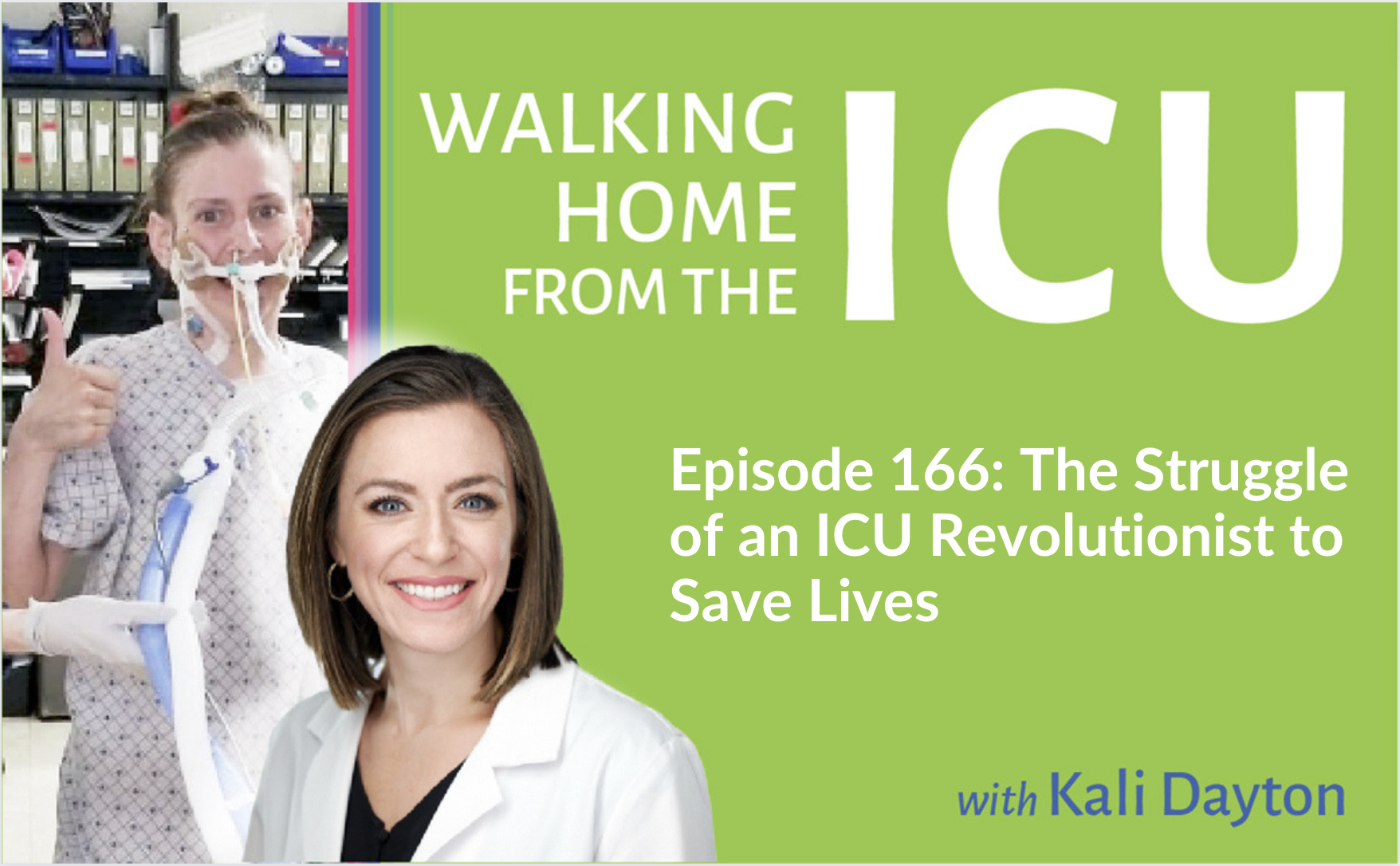
 When patients are so ill that they require a ventilator in the ICU, the antiquated approach of heavy sedation and immobilization should be avoided in order to help prevent the immense burden of physical and cognitive disabilities suffered during survival. To understand this better, listen to Walking Home From The ICU. You will see what ICU consultant Kali Dayton provides to your team. Her training will catalyze changes in your practice to improve outcomes, decrease costs, and allow your patients to return to their full lives. Learn to love your job again as you embrace whole person care instead of caring for inert sedated bodies. Kali is leading ICU teams to become Awake and Walking ICUs through true mastery of the ABCDEF bundle.
When patients are so ill that they require a ventilator in the ICU, the antiquated approach of heavy sedation and immobilization should be avoided in order to help prevent the immense burden of physical and cognitive disabilities suffered during survival. To understand this better, listen to Walking Home From The ICU. You will see what ICU consultant Kali Dayton provides to your team. Her training will catalyze changes in your practice to improve outcomes, decrease costs, and allow your patients to return to their full lives. Learn to love your job again as you embrace whole person care instead of caring for inert sedated bodies. Kali is leading ICU teams to become Awake and Walking ICUs through true mastery of the ABCDEF bundle.
I endorse her mission and look forward to the standardization of this evidence-based approach in ICUs all over the world.
Dr. Wes Ely, author of Every Deep Drawn Breath, leading founder of the ABCDEF bundle and ICU CAM delirium screening tool, and Professor of Medicine in the Division of Allergy, Pulmonary, and Critical Care Medicine at Vanderbilt University Medical Center.